5 May 2022
A Mental Health Crisis Among the Young Is Going Unnoticed
Estimated read time: 5 minutes
In Latin America and the Caribbean, young people’s mental health is in crisis, and the pandemic has only exacerbated the problem. A combination of the pervasive stigma associated with mental illness in many parts of the region and isolation and social and economic tensions brought on by COVID-19 has worsened an issue that is far from new.
The pandemic created a perfect storm of emotional turbulence. As the stress of the virus rocked families, virtual learning, and a fear of getting sick and feeling isolated triggered a rise in anxiety and depression among teenagers.
The prevalence of mental health conditions in Latin America and the Caribbean is 7% in children between 10 and 14 years old and 8% in those aged 15 to 19. The numbers are staggering: 3.3 million girls and 4 million boys in the first group and 4.3 million women and 4.2 million men in the second suffer some form of mental illness. Suicide is the third cause of death in adolescents between 15 and 19 years old (6 in every 100,000 deaths), according to UNICEF’s “State of the World’s Children” 2021 report.
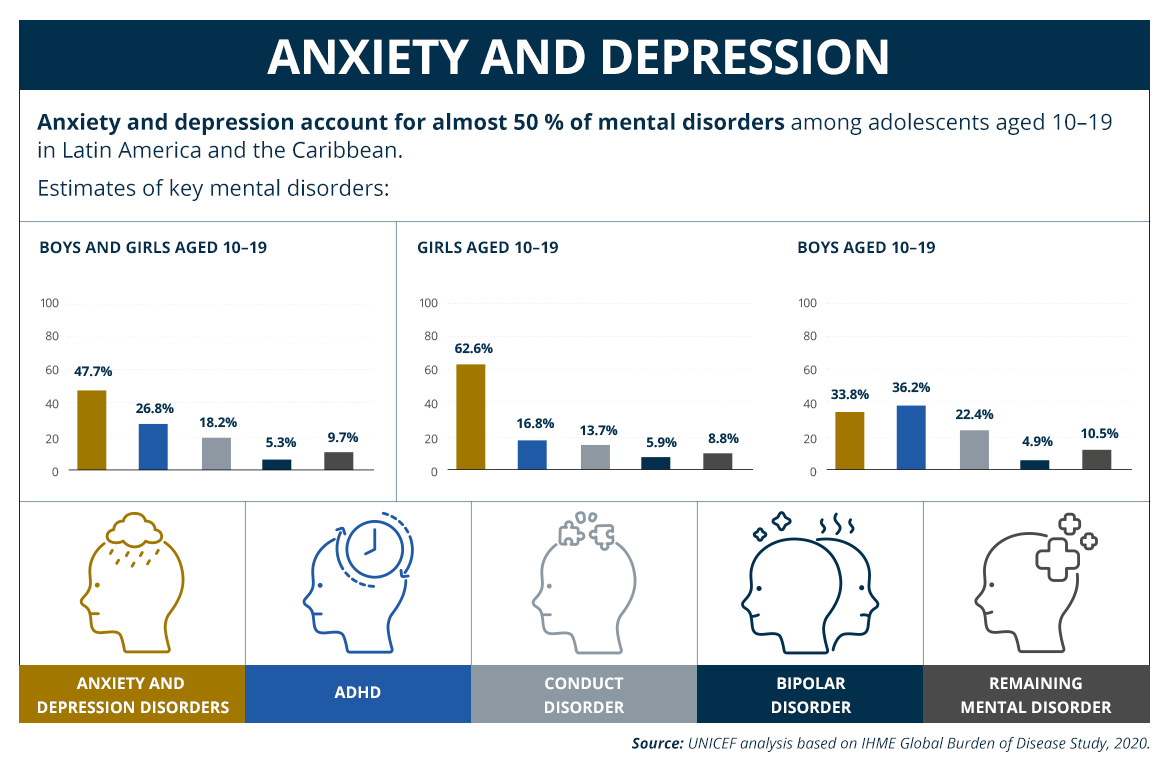
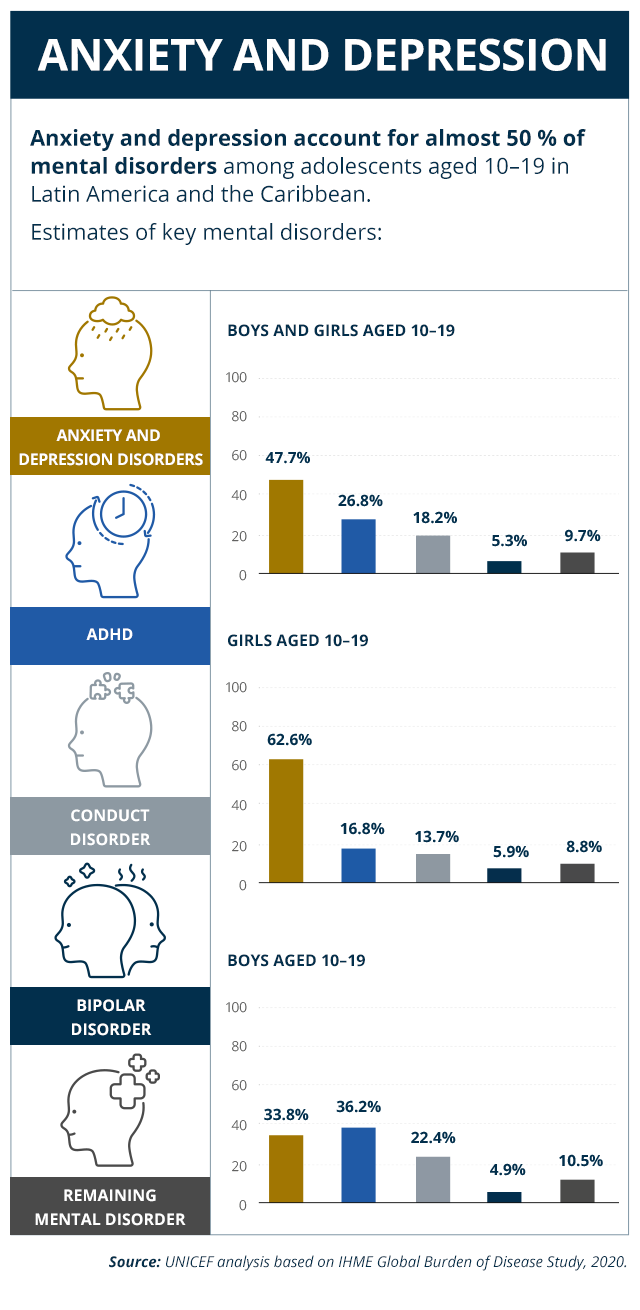
In the region, anxiety and depression represent 50% of all mental health conditions in individuals aged 10 to 19. That statistic is calculated on the basis of cases of young people who received a diagnosis or treatment within the public health system at some point in time, but it omits what some experts call “the silent gap.” Thousands of youths who are in a critical stage in their lives — the transition to adulthood — do not receive a diagnosis and, consequently, are not able to get the counseling or treatment required for full personal and social development.
Anxiety and depression are also the most prevalent among adults, highlighting the importance of early diagnosis and treatment. Mental, neurological and substance-use disorders account for about 20% of the total disability burden, and are second only non-communicable chronic diseases (e.g., cardiovascular disease, diabetes).
More Than Just Sadness and Loneliness
The COVID-19 pandemic radically changed the lives of young people worldwide. Teenagers who rely increasingly on relationships with their peers as they mature were isolated when schools shuttered.
A project called “Activamente, Red Informativa por la Salud Mental” (“Actively, an Informative Network for Mental Health”) looked at the mental health of 750 youth in Colombia, Ecuador, and Argentina in the first year of the pandemic, and detected an increase in symptoms and feelings of anxiety, depression, sadness, hopelessness, powerlessness, loneliness, and fear linked to the crises caused by the coronavirus.
In 1990, Latin American countries signed the Caracas Declaration with the main objective of promoting respect for the human and civil rights of the mentally ill. But more than three decades since its signing, few significant gains have been made. In 2019, treatment gaps still left out 73.5% of adults and 82.2% of youth.
While the U.S. and Canada spend an average of $193.50 per capita on mental health programs and medical care, non-Latin Caribbean countries spend an average of about $24 per capita, and most countries in the Central American and South American regions invest just $1.00 and $2.30 per capita, according to the report Mental Health in Latin America and the Caribbean.
These numbers show that mental health is still thought of as secondary to medical care, evincing a denial at both the public and institutional level.
The lack of a comprehensive strategy to address mental health at the continental, national, and local levels generates conflicts and crises that are worsening over time. The stigma associated with these disorders adds another layer of risk to this emotional time bomb.
The diagnosis and treatment of mental illness among the young remain under-addressed. And mental health stigma doesn’t replicate social or economic disparities: it exists at every level of society. Multiple research studies have examined prejudices associated with mental health and found the following biases to be prevalent:
- Individuals with mental illness are more violent or prone to act impulsively
- They are incapable of getting better
- They are unable to complete tasks such as studying or working
This prejudice toward mental health conditions is pervasive worldwide. In fact, the pejorative use of expressions like “he/she is crazy” in everyday speech reveals the extent to which the stigma is rooted in every aspect of our life, even language.
A profound sense of family is among the positive qualities typically ascribed to Latin American communities. But oddly enough, family can be a negative factor when it comes to talking about mental health. Multiple studies have observed that families tend to deny the existence of mental illness unless symptoms are life-threatening.
Parents and caretakers’ denial of their children’s mental health conditions often constitutes the first barrier to diagnosis, care, and treatment. If it is not overcome, this barrier can not only have social and developmental consequences on a young person, but may also persist into adulthood, when mental illness is typically harder to manage.
Some authors believe that factors such as child abuse and negligence have not been properly examined. Topics like wellness, quality of life, and emotion management during childhood are in the incipient stages of research in Latin America and the Caribbean. Others, like bullying and discrimination, are insufficiently researched. These factors are all linked to mental health.
This is why experts are calling for concrete actions — not just addressing the epidemiology of youth mental illness, but establishing public health programs to end stigma and support parents and caretakers with interventions ranging from medical consultations to care and treatment.
A glimmer of hope can be found in the fact that people are becoming increasingly aware of mental illness, especially younger populations. A study published last December suggests that things are finally beginning to change, and compared with older generations, young people are less likely to stigmatize a mental health condition. Social media and other popular platforms have also made it easier for young people to talk about their experience with mental illness.
Understanding and learning more about a condition are two major steps toward prevention and early diagnosis. But when it comes to mental illness, there is much more individuals and society at large must do to continue heading in the right direction: practice more empathy, compassion, and communication.